Intervention Season 25 Coming Soon to A&E

A&E network’s acclaimed series Intervention is back for a 25th season starting June 3rd. Ken Seeley of Ken Seeley Communities and Intervention911 returns as an interventionist on the Emmy award-winning television show, alongside other esteemed professionals. The show follows those with severe substance abuse and their loved ones as they navigate the reality of addiction. […]
Dangers of Snorting Cocaine

Snorting cocaine has become a deadly gamble with the influx of fentanyl in the cocaine supply. Back in the day, cocaine was that go-to substance that guaranteed a good time. A snort of coke meant you could dance and party for hours. It wasn’t until the long-term effects of cocaine became known that the warning […]
Fentanyl Withdrawal Timeline

Fentanyl is a highly addictive opioid. Get to know what to expect in detox and the fentanyl withdrawal timeline. No other drug is as newsworthy today as fentanyl. This dangerous synthetic opioid has been cited as the cause of a sharp rise in overdose deaths in recent years. Still, many people will abuse this drug […]
Sober Lite is Not Sobriety

What Does Sober Lite Like The Weeknd Mean? Singer The Weeknd has recently caused quite the stir. In his recent interview on GQ Magazine, the singer has claimed that he is living the “sober lite” life. Explaining what he meant by “sober lite” he mentioned that he does drink occasionally and smokes Marijuana. Addiction expert […]
How to Get a Meth Addict Help

Meth use has been rising again in recent years. Learn how to get a meth addict help. Even though it is well known that meth is a dangerous drug, people are still using this synthetic stimulant. Meth subsists of toxic ingredients. These, plus the drug’s impact on the brain, cause a wide range of damage […]
Stages of Withdrawal From Norco
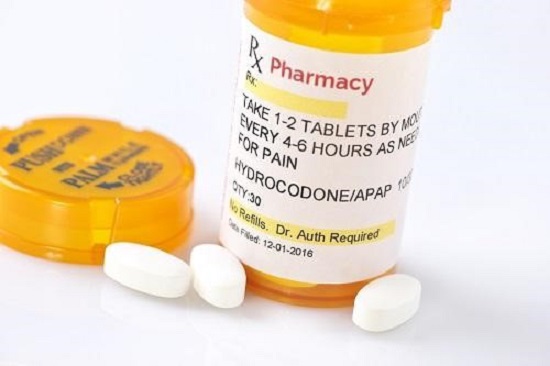
No one enjoys having to suffer from pain of any kind. So, when a doctor prescribes pain pills like Norco (hydrocodone) the drug is welcomed with open arms. Most patients are able to take this drug for a week or so with no problem. But for others, even two weeks on the drug can lead […]
The Problem With the Term “California Sober”

California Sober is Not Sobriety At All Singer Demi Lovato has recently caused quite a stir. In her new documentary called “Dancing with the Devil,” Lovato claims to now be “California sober.” She states that this approach in recovery is better for her than complete sobriety. That abstinence “only sets her up for failure.” Ms. […]
Rates of Alcohol Abuse Rising During COVID-19

People are drinking to relieve boredom and stress during the pandemic. It wasn’t shocking at all when news reports emerged last April that alcohol sales had tripled since the lockdowns started. People were afraid of this unknown, unseen invader. No one knew what was around the next corner, or if they would even have a […]
The Dangers of Skin Abscess from Injecting Heroin

Heroin use has risen in great numbers as opiate abuse exploded in recent years. The intense high that people using synthetic opioids enjoyed has driven people to seek out a cheaper option. This is why heroin use has been on the increase of late. Drug use has increased across all regions and classes. Homeless camps […]
Quitting Alcohol Before It Becomes a Problem
Pay Attention to Your Gut If You Think You Have a Drinking Problem How easy it is to be in a state of denial. Your instincts tell you that you are drinking too much, but your brain refuses to accept it. Instead, you continue drinking more than you should, and even lying about it to […]


